As a woman gets older, the number of viable eggs in the ovary, also known as ovarian reserve, naturally declines. Ovarian activity also declines progressively with age. By the time a woman reaches menopause at age 45 to 55, ovarian reserve and function has diminished, making it almost impossible to get pregnant at this age.
In some women, however, diminished ovarian reserve and impaired ovarian function occur even before 40 years old. This condition is known as primary ovarian insufficiency.
Having ovarian insufficiency is definitely a challenge for women and couples who wish to become pregnant. A diagnosis of ovarian insufficiency prompts women to ask, “Can I still get pregnant?”
Read on to know the answer and to learn more about how ovarian insufficiency affects your fertility journey.
What is ovarian insufficiency?
Primary ovarian insufficiency is a condition that is defined by impaired ovarian function occurring on a continuum with irregular ovulation before the age of 40. This condition can either be transient or progressive, and may ultimately lead to premature menopause, which is menopause that occurs before 40 years old1. Primary ovarian insufficiency is also used to describe related conditions of the ovary, such as hypergonadotropic hypogonadism, ovarian dysgenesis, and premature ovarian failure2.
Women with primary ovarian insufficiency have reduced levels of reproductive hormones and considerable infertility. The resulting infertility is life-changing, especially for those trying to conceive3.
Ovarian insufficiency has been reported in 1 in every 10,000 women by age 20, 1 in every 1000 by age 30, and 1 in 100 women by age 404. Any woman of reproductive age who experiences infertility should be suspected of having primary ovarian insufficiency3.
Causes
For majority of patients diagnosed with primary ovarian insufficiency, the cause is unknown. Some of the proposed underlying causes of ovarian insufficiency are1:
- genetic disorders
- autoimmune disorders
- metabolic disorders
- infections
- iatrogenic or unexplained causes
Genetic disorders that affect the structure of the X chromosome and the development of the ovary are thought to cause ovarian insufficiency. These disorders include X-chromosome disorders such as Turner syndrome, mutations on the X chromosome such as in Fragile X syndrome, gonadal dysgenesis, and mutations in enzymes and hormones required for reproduction.
The most common autoimmune disease linked to ovarian insufficiency is thyroiditis. Other autoimmune diseases that have been associated with the development of ovarian insufficiency include hypothyroidism, myasthenia gravis, systemic lupus erythematosus, and rheumatoid arthritis.
Abnormalities and mutations in enzymes involved in metabolic pathways have also been linked to ovarian insufficiency. Metabolic disorders such as galactosemia, carbohydrate-deficient glycoprotein deficiency, and deficiencies in enzymes crucial in estrogen production, such as aromatase and 17-α-hydroxylase.
Infections such as mumps and HIV have also been studied as probable causes of ovarian insufficiency. Meanwhile, proposed iatrogenic causes of ovarian insufficiency include chemotherapy and radiotherapy.
Symptoms
Primary amenorrhea, which is the absence of menses at 16 years old, is the first symptom in 10% of women diagnosed with primary ovarian insufficiency. In majority of patients, however, the presenting symptom is irregular menstrual cycles, described as any of the following5:
- absence of periods
- infrequent menstrual periods, <6 or 8 periods every year
- heavy menstrual bleeding
- short menstrual cycles
- irregular bleeding
Symptoms of low estrogen levels are also present, such as1,2:
- hot flashes
- night sweats
- mood swings
- sleep disturbance
- thinning and drying of the vaginal wall, also known as atrophic vaginitis
Women with primary ovarian insufficiency eventually experience infertility. In many cases, the diagnosis is made after evaluation for irregular menses. Still, there are cases when the diagnosis is only made after evaluation for infertility3.
Aside from these symptoms, women with ovarian insufficiency may also experience other health conditions that are associated with low estrogen levels, such as osteoporosis, cardiovascular disease, and neurocognitive disorders such as dementia6.
How is ovarian insufficiency diagnosed?
Primary ovarian insufficiency is diagnosed based on the presence of the following criteria2:
- age below 40 years old
- absent or infrequent periods
- 2 elevated levels of follicle-stimulating hormone (FSH), taken at least one month apart
FSH is a hormone synthesized in the anterior pituitary and is a key hormone for estrogen production and follicle development in females. Increased levels of FSH in females are associated with ovarian dysfunction. For example, in premature ovarian failure, FSH levels remain elevated because of the absence of negative feedback from the ovaries7.
Women being evaluated for ovarian insufficiency should be asked about their detailed menstrual history. The doctor should take note of the possible causes of abnormal menstrual cycles, such as polycystic ovarian syndrome, chronic illnesses such as diabetes or celiac disease, thyroid disorders, pituitary lesions, and even pregnancy. Family history, particularly genetic and autoimmune diseases, should be considered. A thorough physical examination focusing on the examination of body habitus and the female genital tract can help in making the diagnosis1.
Aside from detection of FSH levels, other tests requested during diagnosis may include the following2,5:
- Karyotype analysis
Karyotyping helps identify whether monosomy X, or Turner syndrome (45,X) is present. Turner syndrome presents with underdeveloped reproductive organs, making it a probable cause of primary ovarian insufficiency. A study also reported that genes that are important for sexual development may be inactivated in the normal X chromosome of patients with Turner syndrome8.
- Detection of mutation in the FMR1 gene
Females suspected of having ovarian insufficiency may be tested for the presence of FMR1 gene mutation. Mutation in the X-linked FMR1 gene results in Fragile X syndrome, which is the number 1 genetic cause of cognitive disability. Studies have shown that females with Fragile X syndrome have up to 23% incidence rate of primary ovarian insufficiency1. Fragile X-associated ovarian insufficiency presents as abnormal follicle function9.
- Detection of adrenal antibodies via immunoprecipitation or indirect immunofluorescence
About 4% of women with ovarian insufficiency have adrenal antibodies. A positive test for adrenal antibodies suggests that the ovarian disorder is due to autoimmune processes that involve steroidogenic cells and lymphocytes10.
- Pelvic ultrasound
A pelvic ultrasound will help identify the presence of cysts in the ovaries, which is a prominent feature of women with deficiency in the enzyme 17,20-desmolase, an important enzyme for the formation of the female hormones 17-hydroxyprogesterone and 17-hydroxypregnenolone. Multiple cysts in the ovary are also present in autoimmune oophoritis and polycystic ovary syndrome, which are probable underlying causes of primary ovarian insufficiency10.
- Bone mineral density
Ovarian insufficiency is a risk factor for the development of bone11. Evaluation of bone mineral density helps in assessing the risk and identifying the presence of osteoporosis and other bone diseases. Early identification is important in preventing long-term complications of decreased bone health5.

«Many modern treatment options for ovarian failure already exist.»
Can I still get pregnant if I have ovarian insufficiency?
Yes, you can still get pregnant even if you have been diagnosed with ovarian insufficiency. In some women, normal ovarian function resumes even without treatment, thus allowing pregnancy12. Reports reveal that approximately 5 to 10% of women were able to naturally conceive and deliver a baby even after being diagnosed with the condition2.
Still, a vast majority of women with ovarian insufficiency experience infertility. Inability to conceive causes not only physical stress, but also considerable emotional stress to women and their partners.
Fortunately, several strategies that promote pregnancy in the setting of ovarian insufficiency are now available. With a wider set of treatment options, new fertility modalities provide hope for women desiring of pregnancy.
Treatment for ovarian insufficiency
The following are the treatment options currently recommended for women with ovarian insufficiency who are desirous of pregnancy13:
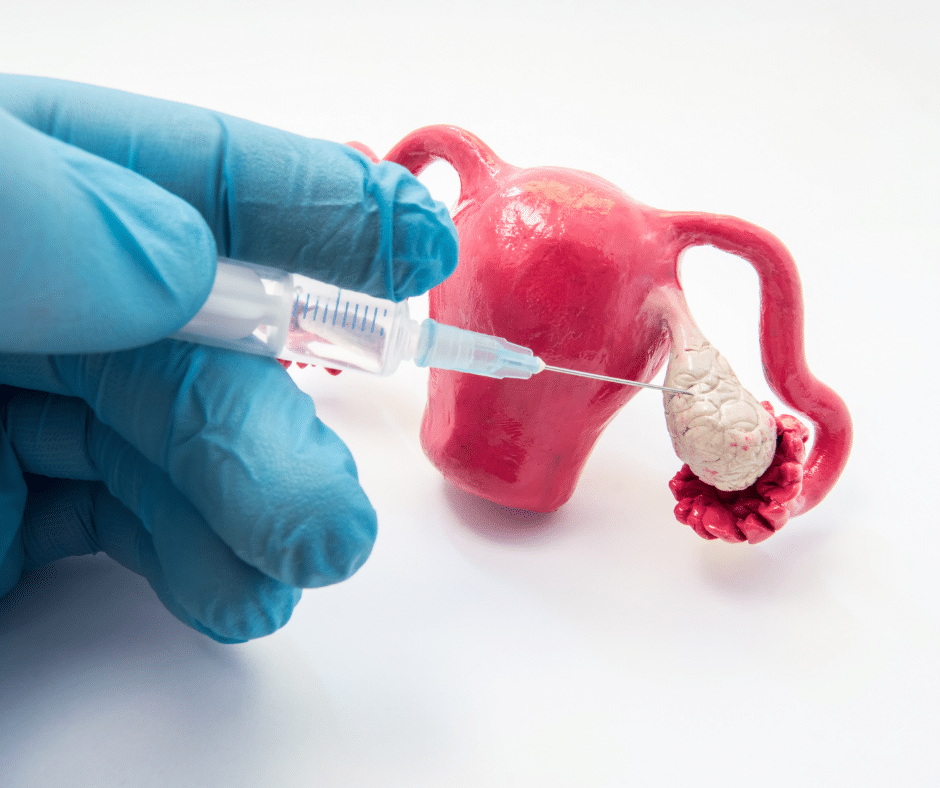
- Oocyte donation
Oocyte donation is the preferred treatment for women with ovarian insufficiency who want to get pregnant13. Oocyte donation involves a female donor and the female recipient who wishes to conceive. Unlike sperm donation, oocyte donation is an invasive procedure that involves surgical retrieval of mature oocytes from the ovaries of the donor, who is put under local anesthesia14. In the United States, oocyte donation makes up about 10% of all assisted reproductive technology (ART), with more than 50% live birth rate every cycle15.
- Hormone replacement therapy (HRT)
HRT is a common treatment approach for primary ovarian insufficiency. The aim of HRT is to restore normal estrogen levels in women. It is recommended that HRT be started at the time of diagnosis of primary ovarian insufficiency until menopause16. A sample HRT regimen is daily 50-100 μg transdermal estradiol, which is a form of estrogen, supplemented with 5-10 mg of medroxyprogesterone acetate for 12 days per month1.
HRT, combined with ovarian stimulation, has resulted in a huge number of pregnancies13. HRT also provides protection against diseases linked to ovarian insufficiency, such as osteoporosis, cardiovascular diseases, dementia, and genitourinary syndrome16.
- Ovarian stimulation
Ovarian stimulation involves the administration of key female hormones, such as FSH and luteinizing hormone (LH) above normal levels. This allows the maturation of multiple oocytes, which can then be retrieved during each IVF cycle. The oocytes can then be used for embryo culture, embryo transfer, and implantation. Spare embryos may also be cryopreserved to increase chances of future pregnancies, without the need for another round of ovarian stimulation and retrieval of oocytes17.
A relatively new modality in promoting pregnancy in women with ovarian insufficiency is the use of DHEA. DHEA was shown to improve the ovarian environment, promote estrogen and progesterone production, and increase the number of receptors for FSH. These effects result in the growth of more pre-antral and small antral follicles. Multiple studies have reported that DHEA administration resulted in enhanced ovulation and successful pregnancies13.
Aside from these techniques, two new emerging technologies are being explored to increase fertility rates in women with ovarian insufficiency13:
- In vitro activation (IVA)
Women diagnosed with primary ovarian insufficiency may have irregular or absent menstrual cycles, but they still have dormant follicles in the ovaries. IVA rescues these residual dormant follicles by manipulating the processes involved in their maturation. IVA therefore helps women become pregnant using their own egg cells18.
- Stem cell therapy
Stem cell injection has also been explored recently as a means to induce pregnancy in women with ovarian insufficiency. A recent study showed that injection of umbilical cord mesenchymal stem cell to the ovaries plus HRT resulted in 2 pregnancies out of 14 women who participated in the study19.
Can ovarian insufficiency be prevented?
Primary ovarian insufficiency that is caused by genetic or autoimmune disorders may be impossible to prevent, but it is possible to predict whether other relatives would also present with ovarian insufficiency. Genetic analysis and family studies can help identify family members who are at risk of having ovarian insufficiency.
Meanwhile, primary ovarian insufficiency due to chemotherapy or radiotherapy may be prevented by considering other therapeutic options, especially for women who strongly desire to become pregnant. If there are no other options, patients could opt for cryopreservation of oocytes prior to chemotherapy or radiotherapy.
References
- Cox, L. and Liu, J. (2014). Primary ovarian insufficiency: an update. International Journal of Women’s Health. 6:235-243.
- Nelson, L. (2009). Primary Ovarian Insufficiency. N Engl J Med. 360(6):606-614.
- Piedade, K., Spencer, H., Persani, L., and Nelson, L. (2021). Optimizing Fertility in Primary Ovarian Insufficiency: Case Report and Literature Review. Front Genet. 12:676262.
- Coulam, C., Adamson, S., and Annegers, J. (1986). Incidence of premature ovarian failure. Obstet. Gynecol. 67(4):604-6.
- Rafique, S., Sterling, E., and Nelson, L. (2012). A New Approach to Primary Ovarian Insufficiency. Obstet Gynecol Clin North Am. 39(4):567-586.
- McKinlay, S., Brambilla, D., Posner, J. (1992). The normal menopause transition. Maturitas. 14:103-115.
- Orlowski, M. and Sarao, M. (2021). Physiology, Follicle Stimulating Hormone. In: StatPearls [Internet]. Treasure Island (FL). StatPearls Publishing.
- Willard, H. (2001). The sex chromosomes and X chromosome in activation. In: Scriver, C., Beaudet, A., Sly, W., et al. The Metabolic and Molecular Bases of Inherited Disease. NY, USA: McGraw-Hill.
- Fink, D., Nelson, L., Pyeritz, R., Johnson, J., Sherman, S., Cohen, Y., and Elizur, S. Fragile X Associated Primary Ovarian Insufficiency (FXPOI): Case Report and Literature Review. Front. Genet. 9:529.
- Bakalov, V., Anasti, J., Calis, K., Vanderhoof, V., Premkumar, A., Chen, S., Furmaniak, J., Smith, B., Merino, M., Nelson, L. (2005). Autoimmune oophoritis as a mechanism of follicular dysfunction in women with 46,XX spontaneous premature ovarian failure. Fertil Steril. 84(4):958-65.
- Popat, V., Calis, K., Vanderhoof, V., Cizza, G., Reynolds, J., Sebring, N.., Troendle, J., Nelson, L. (2009). Bone mineral density in estrogen-deficient young women. J Clin Endocrinol Metab. 94(7):2277-83.
- Kalantaridou, S., and Nelson, L. (2000). Premature Ovarian Failure Is Not Premature Menopause. Annals New York Academy Sciences. 900:393-402.
- Fraison, E., Crawford, G., Casper, G., Harris, V., and Ledger, W. (2019). Pregnancy following diagnosis of premature ovarian insufficiency: a systematic review. RBMO. 00(0):1-10.
- Baetens, P., Devroey, P., Camus, M., Van Steirteghem, A., and Ponjaert-Kristoffersen, I. (2000). Counselling couples and donors for oocyte donation: the decision to use either known or anonymous oocytes. Human Reproduction. 15(2):476-484.
- Melnick, A. and Rosenwaks, Z. (2018). Oocyte donation: insights gleaned and future challenges. Fertility and Sterility. 110(6):988-993.
- Machura, P., Grymowicz, M., Rudnicka, E., Pieta, W., Calik-Ksepka, A., Skorska, J., an Smolarczyk, R. (2018). Premature ovarian insufficiency – hormone replacement therapy and management of long-term consequences. Prz Menopauzalny. 17(3):135-138.
- Farquhar, C., Marjoribanks, J., Brown, J., Fauser, B., Lethaby, A., Mourad, S., Rebar, R., Showell, M., and van der Poel, S. (2017). Management of ovarian stimulation for IVF: narrative review of evidence provided for World Health Organization guidance. RBMO. 35:3-16.
- Huhtaniemi, I., Hovatta, O., La Marca, A., Livera, G., et al. (2018). Advances in the Molecular Pathophysiology, Genetics, and Treatment of Primary Ovarian Insufficiency. Trends in Endocrinology & Metabolism. 29(6):400-419.
- Ding, L., Yan, G., Wang, B., Xu, L., Gu, Y., et al. (2018). Transplantation of UC-MSCs on Collagen Scaffold Activates Follicles in Dormant Ovaries of POF Patients with Long History of Infertility. Science China Life Sciences. 2:1554-1565.